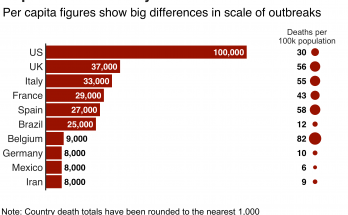
COVID Vaccinated Made Up 42% of January and February fatalities
According to nationwide data from the Centers for Disease Control and Prevention, the COVID vaccinated made up 42% of fatalities in January and February 2022. This is during the highly contagious omicron variant’s surge, compared with 23% of the dead in September, the peak of the delta wave. What does this tell us? It tells us that with or without a vaccination, everyone should continue to wear a mask and exercise social distancing.
COVID-19 Mask Guidelines Revised—Again
Here is a great article written by Kathy Katella for Yale Medicine [Originally published: July 28, 2021. Updated: April 20, 2022]
As the numbers of COVID-19 deaths have dropped, the Centers for Disease Control and Prevention (CDC) loosened its guidance around masks for the second time this year. The latest recommendations allow roughly 70% of people in the United States to remove their masks if they want—indoors as well as outdoors. The guidelines suggest many Americans no longer need to maintain a social distance or avoid crowded indoor spaces.
Whether or not you fall into the 70% depends on where you live—the CDC’s system classifies counties as being low, medium, or high risk, based on such data as hospital beds being used, hospital admissions, and total number of new COVID-19 cases per 100,000 people in an area in the previous week. You can check the risk in your county using a tool on the CDC website.
- If you live in a low-risk county: Wear a mask based on your personal preference, informed by your personal level of risk.
- If you live in a medium-risk county: If you are immunocompromised or at high risk of severe illness, talk to your healthcare provider about whether you need to wear a mask and take additional precautions. If you live or have social contact with someone at high risk for severe illness, consider testing yourself for infection before you get together and wearing a mask when indoors with them.
- If you live in a high-risk county: Wear a well-fitting mask indoors in public, regardless of vaccination status or individual risk (including in K-12 schools and other community settings). Additional precautions may be needed for people at high risk for severe illness.
Wherever you live, the CDC recommends staying up to date with your COVID-19 vaccines and getting tested if you have symptoms. As the result of a court order in April, it is no longer required to wear masks on public transportation conveyances and at transportation hubs, although the CDC continues to recommend people wear masks in indoor public transportation settings at this time. It’s also important to avoid crowded spaces and poorly ventilated indoor spaces if you are at increased risk of getting very sick from COVID-19, and to stay at least six feet away from other people if you are at high risk or not up to date on your vaccines.
The guidelines came a month after CDC recommendations in January, when Omicron was surging, that provided specifics on the types of masks and respirators that can be used to prevent transmission of SARS CoV-2, the virus that causes COVID-19. They specified that some types of masks and respirators, such as N95s and KN95s, provide more protection than others, but advised wearing the most protective mask that fits well and that you will wear consistently.
The recommendations aren’t set in stone. If a threatening new variant emerges, the CDC could recommend wearing masks again.
“There is still a lot we don’t know, especially as the new variants continue to emerge,” says Carlos Oliveira, MD, PhD, a Yale Medicine pediatric infectious diseases specialist. In Spring 2021, when the virus seemed to be waning, Dr. Oliveira had recommended people hold on to their masks in case they needed them again, which they did when the Delta variant surged that summer. “There could be spikes in [coronavirus] transmission for a variety of reasons,” he said.
Sheela Shenoi, MD, MPH, a Yale Medicine infectious diseases specialist, also held onto her masks at that time, even though the U.S. as a whole was making progress in vaccinations. “I hesitate to say that we are approaching a post-COVID world when so many are still being ravaged by this virus,” she said. “If there is anything we should have learned, it is that we are all interconnected; what happens in one part of the world affects everybody.”
Dr. Shenoi said, “There’s nothing that’s ‘safe’—it’s always ‘safer.’ If you are fully vaccinated, it is safer than it was two years ago to be around people without a mask,” she said.
The doctors also expressed concern for people who are at risk for complications if they do get infected, including those who are older or immunocompromised, and children younger than 5 who are still not eligible for the vaccines. Dr. Oliveira suggested parents do whatever they can to limit a child’s exposure to unvaccinated people. “My advice—if your children can’t get the vaccine—is to make sure they are with immunized people outside of school,” he said. “Try to get everyone in the family who can get the vaccine to get it.”
You might still wear a mask to protect yourself during cold and flu season
Masks have been a valuable preventive tool throughout the pandemic, and some health experts have pointed out that COVID-19 is not the only reason to hold onto them.
Cases of respiratory syncytial virus (RSV), a common respiratory virus that can be serious in children, immunocompromised people, and older adults, ticked upwards in some places in the U.S. last year. “It’s problematic because we are still in the COVID-19 mindset, so anyone who is sneezing or has a runny nose may think they need to get tested for COVID-19,” said Dr. Shenoi at the time. “It’s particularly hard for parents. Under normal circumstances—before COVID-19—kids would have a sniffle going on from November to March, and we knew to expect that.”
Karen Jubanyik, MD, a Yale Medicine emergency medicine specialist, urges adults to consider wearing masks during flu season if they are at risk for or interact with people who are vulnerable to complications from the flu. “Because the flu hits you all of a sudden—you may feel fine even though you are potentially contagious, then all of a sudden you have a fever of 102,” she says.
Making a personal choice about masks
Wearing a face mask has been a topic of debate among some Americans; however, masks are part of the culture in some Asian countries, where people wear them to protect from circulating viruses like the flu. The habit took hold after those countries were hit hard by severe acute respiratory syndrome (SARS), which led to more than 8,000 infections and almost 800 deaths in 2002-2003.
Mask mandates, which have been part of the COVID-19 infection prevention strategy at local, state, and national levels, have not been popular among everyone in the U.S., where individualism prevails. “I’m not sure it has sunk in how interconnected we are—that what one person does affects the next person, affects the neighborhood, affects two people down the chain—and all that can have consequences,” Dr. Shenoi says.
At the same time, maybe COVID-19 has led some Americans to think about masks in a new way, Dr. Shenoi adds. This could be a helpful attitude if the CDC finds it necessary to change its recommendations again—in favor of masks. “Now that we’ve lived through this, I think masks are much more familiar to us. We know how easy it is—how straightforward it is—to wear a mask. We’ve learned that this is doable.”
Original Source: https://www.yalemedicine.org/news/cdc-mask-guidance